When lung volumes are measured in a plethysmograph the actual measurement is called the Thoracic Gas Volume (TGV). This is the volume of air in the lung at the time the shutter closes and the subject performs a panting maneuver. Ideally, the TGV measurement should be made at end-exhalation and should be approximately equal to the Functional Residual Capacity (FRC). For any number of reasons in both manual and automated systems this doesn’t happen and the point at which the TGV is measured is either above or below the FRC.
Testing software usually corrects for the difference in TGV and FRC by determining the end-exhalation baseline that is present during the tidal breathing at the beginning of the test. Using this value the software can determine where the TGV was measured relative to the tidal breathing FRC and then either subtracts or adds a correction factor to derive the actual FRC volume.
One problem with this is that leaks in either the subject or the mouthpiece and valve manifold can occur during the panting maneuver and the end-exhalation baseline can shift and this will affect the calculation of RV and TLC. I’ve discussed this previously and as a reminder, RV is calculated from:
RV = [average FRC] – [average ERV]
where the FRC is determined from the corrected TGV and ERV is determined from SVC maneuvers. TLC is then calculated from:
TLC = RV + [largest SVC]
When the post-shutter FRC baseline shifts upwards (higher lung volumes relative to the pre-shutter FRC):
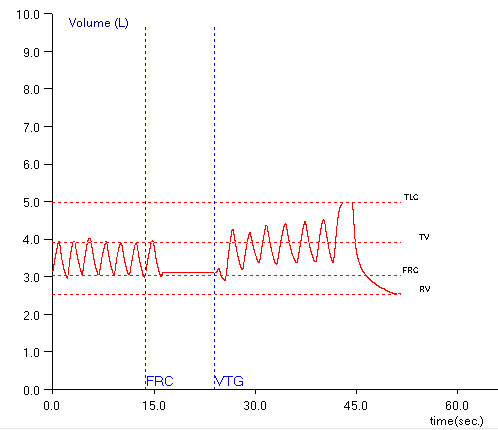
ERV is underestimated, which in turn causes both RV and TLC to be overestimated. When the post-shutter FRC baseline shifts downwards (lower lung volumes relative to the pre-shutter FRC):
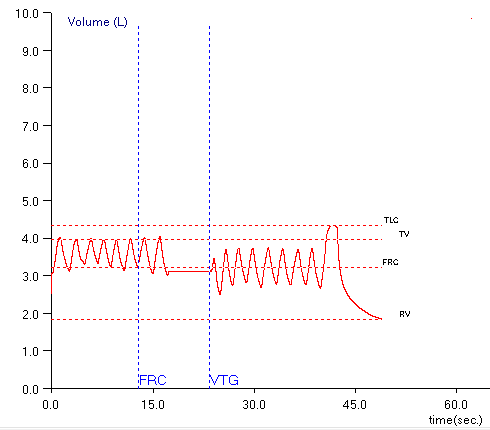
ERV is overestimated, which in turn causes both RV and TLC to be underestimated.
I’ve been aware of this problem for quite a while and use this as a guideline when selecting the FRCs and SVCs from specific plethysmograph tests. All of these assumptions are based on the fact that FRC is derived from the pre-shutter end-exhalation tidal breathing. Well, you know what they say about assuming…
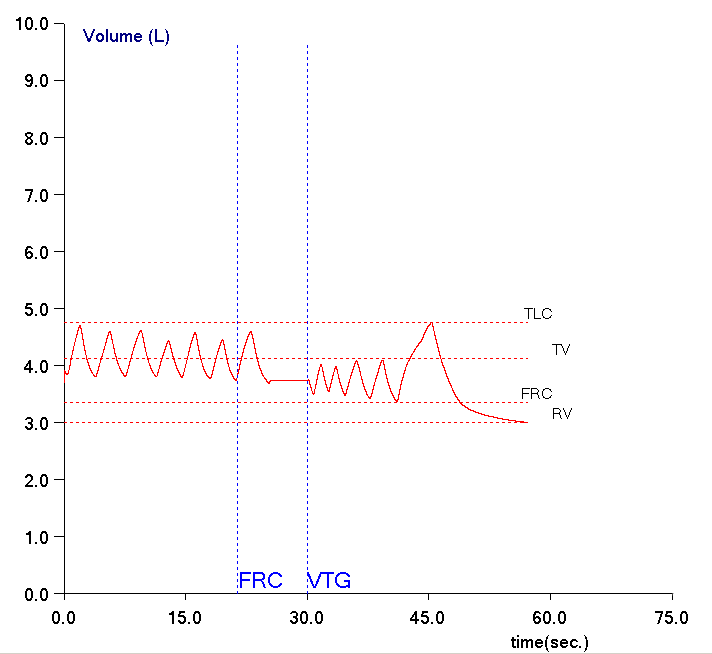
Our lab software was updated a while back, ostensibly with only the changes we needed to perform electronic signing by the pulmonary physicians. I’ve reviewed the information we got concerning the update and there is nothing in it that indicates that any changes were made in any of the testing modules. Recently I was reviewing the plethysmographic lung volume for a patient and suddenly realized that the FRC baseline was being determined by the post-shutter end-exhalation level.
In this particular instance this means is that even though the shutter closed near the end-exhalation level of the pre-shutter tidal breathing, the reported FRC was being corrected to a much lower lung volume. This was causing both RV and TLC to be underestimated. Interestingly, for this patient their TGV measurements were well within +/- 5% (the 2005 ATS/ERS standard for plethysmographic FRC measurements), but the FRCs were not and this was all due to post-shutter baseline shifts.
Fortunately, our software lets me mix and match SVC and TGV results, and to manually correct the FRC. This allowed me to take the highest quality TGV measurements and correct the FRC and then to match them with the highest quality SVC measurements (also corrected for FRC). So for this patient I was able to report what I believe to be reasonably accurate lung volume measurements.
But just to keep me confused, a couple of reports later another patient had also had their lung volumes measured plethysmographically, and also had a post-shutter baseline shift in FRC, but this time the software was using the pre-shutter end-exhalation level to determine FRC (and yes, there was a negative ERV).
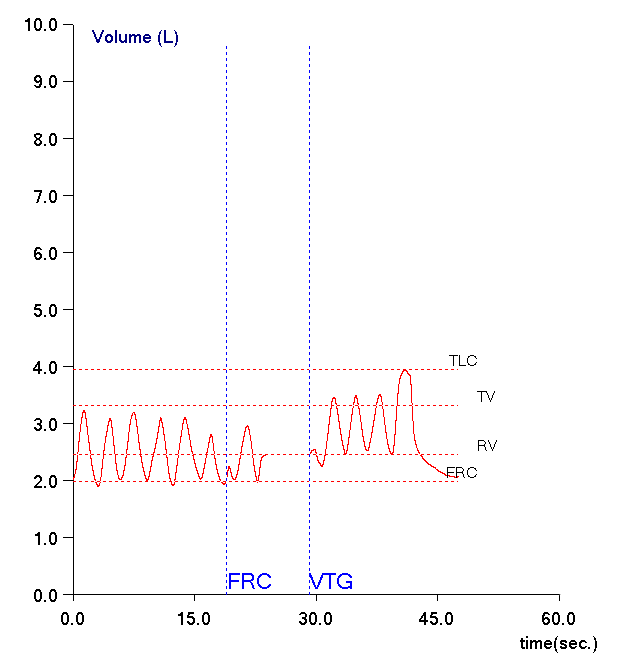
Looking carefully at all the plethysmographic lung volumes I’ve reviewed since then I’ve seen that FRC is being determined occasionally by the post-shutter end-exhalation level and more often by the pre-shutter end-exhalation level. I haven’t been able to determine why one or the other is being used so I have no idea what criteria the software is using.
Other than mentioning that the SVC maneuver should be linked to the FRC measurements there are no guidelines in the ATS/ERS 2005 lung volume standards as to how this linking should be done. Although it would seem to be more logical for the pre-shutter end-exhalation level to be used to determine FRC (since they appear to be more closely related to the actual TGV measurement) this is left to individual manufacturers.
Note: I will also mention that there are no guidelines for the number of tidal breaths and the repeatability of the end-exhalation volumes that are used to determine FRC and this is also left to the individual manufacturers.
In a sense, the real problem is that leaks are occurring while the shutter is closed. I suspect that it’s the patients that are leaking rather than the valve manifold because leaks don’t occur with every patient or with every test (although that doesn’t rule out an intermittent valve problem). It’s hard to know how to address this since we routinely instruct the patients to keep their lips tight and we already use the largest mouthpiece the patient is comfortable using.
Baseline shifts are more often downwards than they are upwards. This implies that leaks are more likely during the compression (exhalation) part of the panting maneuver but I suspect that this is because patients probably don’t generate as much negative pressure as they do positive pressure during panting.
Regardless of where or when the leak is occurring it’s also unclear to me what effect a leak has on the actual TGV measurement. A leak will cause lung volume to change during the panting period and may also dampen the amplitude of the mouth pressure signal but I suspect that these effects are small. Our plethysmographs accumulate between 1 and 4 pants for a TGV measurement but any difference between individual pants (other than the normal pant-to-pant variations) in patients with baseline shifts is not readily apparent.
We maintain our plethysmographs well and try to instruct our patients properly but leaks and baseline shifts during plethysmographic lung volume measurements still happen. For these reasons I suspect that this is not an uncommon problem regardless of which manufacturer’s equipment is being used. How evident this problem is however, depends on the way each manufacturer’s software displays the TGV results graphically and I’ve seen examples from some systems where a baseline shift would be difficult to detect.
As importantly, our ability to detect a baseline shift also depends on the procedure we follow. Specifically, for my lab a TGV test consists of:
- tidal breathing
- shutter closes
- panting
- shutter opens
- tidal breathing
- SVC maneuver
I’ve seen results from labs where the subject goes directly into an SVC maneuver as soon as the shutter opens and without a second period of tidal breathing a baseline shift would probably be hard to detect.
Strictly speaking the periods of tidal breathing pre-shutter and post-shutter serve different purposes. Pre-shutter the end-exhalation level of tidal breathing is used to determine where FRC is in relation to the TGV. Post-shutter the end-exhalation level is used to determine IC and ERV from the SVC maneuver. I would like to see these facts addressed the next time the ATS/ERS updates the standards for lung volume measurements and that pre-shutter and post-shutter tidal breathing periods be mandated and FRC determined independently for both.
Our software (and I suspect those from many other manufacturers as well) assumes that the pre-shutter tidal end-exhalation level is the same as post-shutter (ore vice-versa). It’s clear that this isn’t always true and that when it isn’t it can affect the reported RV, FRC and TLC. So you know what they say about assuming…
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Standardisation of the measurement of lung volumes. Eur Respir J 2005; 26: 511-522.