I’ve mentioned before that my lab’s database goes back to 1990, so we now have 27 years of test results available for trending. At least a couple times a week we have a patient who was last seen 10 or even 20 years ago. When I review their results I try to see if there has been any significant change from their last tests. Since the last tests are often quite some time in the past the changes in an absolute sense are often noticeably large. The question then becomes whether or not these changes are normal.
Although the ATS/ERS, NIOSH and ACOEM standards for spirometry address changes over time they don’t specifically discuss changes over a decade or longer. Instead, without indicating a time period (other than saying a year or more), the concensus is that a change greater than 15% in age-adjusted FVC or FEV1 is likely to be significant. A change in absolute values greater than:
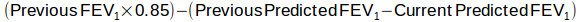
Or if the current FEV1 is less than:
Then the change is likely significant.
This sounds fairly reasonable and although we could quibble about the importance of how quickly or slowly this age-adjusted 15% change occurs and how well it applies when the patient’s latest age is beyond the reference equation’s study population (we have a fair number of 90+ year old patients nowadays) or when it’s across a developmental threshold (adolescent to adult), it’s still a good starting point.
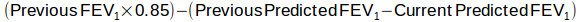
I’ve been more or less following these rules for the last several years, when the results for a patient whose last test was 18 years ago came across my desk. The FEV1 from the current spirometry was 71% of predicted and the FEV1 from 18 years ago was 70% of predicted. Strictly speaking the absolute change was about -15% (the FEV1 was 2.06 L in 1999 and 1.76 L in 2017, a 0.30 L change) but when adjusted for the change in age, that’s only 40% what a significant change would need to be:
Given that the FEV1 percent predicted from both the older and newer test were essentially identical I automatically started to type “The change in FEV1 is normal for the change in age” when it suddenly occurred to me that neither FEV1 was normal in the first place so how could I be sure the change be normal?
The first problem is that we don’t know what’s happened in between the two tests. The original spirometry test showed mild airway obstruction, but in the interim it could have been well controlled and normal the entire time. It could also be that the only reason that they’re seeing a pulmonary physician is that they are having an exacerbation and that it’s actually just chance that the FEV1 percent predicted is the same between the two tests.
The second problem is that the way that the ATS/ERS, NIOSH and ACOEM assess changes over time come from occupational studies where the individuals studied were presumably normal to begin with and where the changes that occurred were expected to be due to occupational exposures. This may mean that it’s possible that we can use their criteria for change only when the baseline test was normal. When a patient has a lung disorder, regardless of whether it is obstruction or restriction, it isn’t clear at all that there is such a thing as a normal change over time. In fact an accelerated decline in FVC or FEV1 is actually the “norm” for certain lung diseases (i.e. COPD and IPF) and that means a change less than that (although probably acceptable to the individual in question) isn’t, strictly speaking, normal.
This just may all be just an issue of semantics, however. Saying that a change isn’t significant (which is what the ATS/ERS, NIOSH and ACOEM standards are saying) isn’t the same as saying that it’s a normal change. That means there’s no reason not to say “the change in FEV1 isn’t significant”. My problem with this is that although it may be be statistically and semantically correct to say this it also somehow seems to be lacking in information content.
And it’s also probably misleading. If the patient’s FEV1 had decreased from 2.06 L (70% of predicted) by 0.76 L to 1.30 L (52% of predicted), that would be less than a significant change by the ATS/ERS, NIOSH and ACOEM criteria, but it would also be a change from mild airway obstruction to moderately severe airway obstruction and I’m hard pressed not to think that’s significant. The problem is that the formula is dominated by the predicted normal values and this means a significant change has to be relatively large in an absolute sense and for this patient based on her initial FEV1, anything less than 0.77 L over 18 years would not be significant. This makes some sense if the FEV1 was originally normal, but if the FEV1 is already compromised then even small changes may be clinically significant.
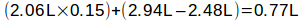
There needs to be some kind of middle ground here. I think it’s important to give an indication whether a change over a prolonged period of time is normal or abnormal and as a first approximation the ATS/ERS, NIOSH and ACOEM consensus is a reasonable approach. Where I think it tends to fail is in patients with severe reductions in FVC or FEV1. One possible way to correct this lies in the recognition that FVC and FEV1 have a floor, i.e. a lower limit beyond which mortality increases dramatically. For FEV1 at least this appears to be about 0.50 L so an amended formula could look something like this:
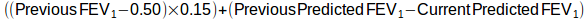
For this patient this would change the acceptable change over 18 years from 0.77 L to 0.69 L. Not a big change, but for somebody that already had a severe decrease in FEV1 it lowers the threshold for what constitutes a significant change.
This still doesn’t get around the fact that we don’t know what happened in the interim but realistically this is a problem no matter what time frame that tests occur. We’re likely to place more reliance on trends when testing is performed more frequently, but we still have to admit our ignorance of what happens between tests no matter how often they are performed.
Note: This is why I don’t like graphical trend reports that draw lines between data points. The line implies what is happening in between tests and that’s just sheer conjecture.
At the moment I think I’ll use my amended formula when trying to assess whether a change over a prolonged period of time is within normal limits. At the same time though, even if the change isn’t statistically significant but there is a significant change in diagnosis (i.e. say from mild obstruction to severe obstruction) then it’s probably worth stating that the change “is larger than expected for the change in age”. Saying that may not be statistically correct but it’s certainly correct in a clinical sense.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of lung function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.
Townsend, MC. ACOEM Guidance Statement. Spirometry in the occupational health setting – 2011 update. J Occup Env Med 2011; 53(5): 569-584
U.S. Department of Health and Human Services. Public Health Service. Centers for Disease Control. National Institute for Occupational Safety and Health. Education and Information Division. Criteria for a recommended Standard. Occupational Exposure to Respirable Coal Mine Dust. 1995.