The FEV1 and VC both provide quite different information about a patient’s lungs. Unfortunately, spirometry as it is currently practiced is optimized towards generating an accurate FEV1 more than an accurate VC. This is partly due to limitations in the maneuver itself and partly due to the lack of accurate end-of-test criteria for an adequate VC. In one sense this is okay since more than one person that I’ve known and respected has said that “it’s all about the FEV1”.
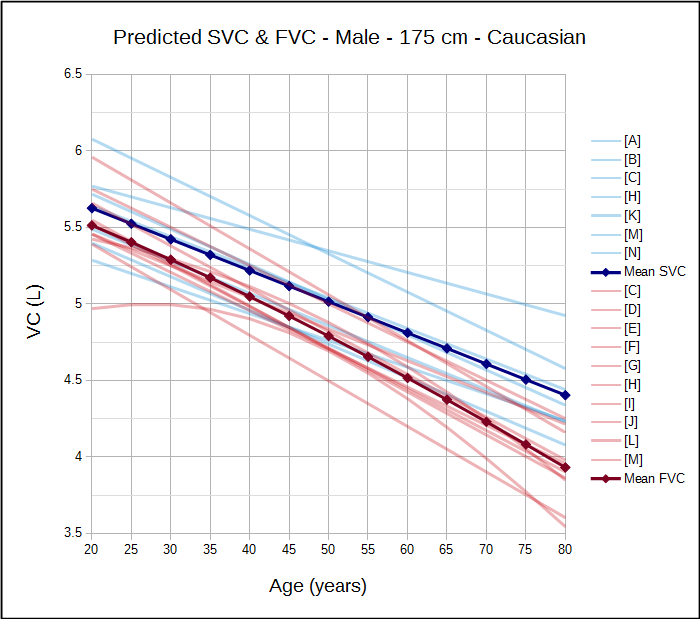
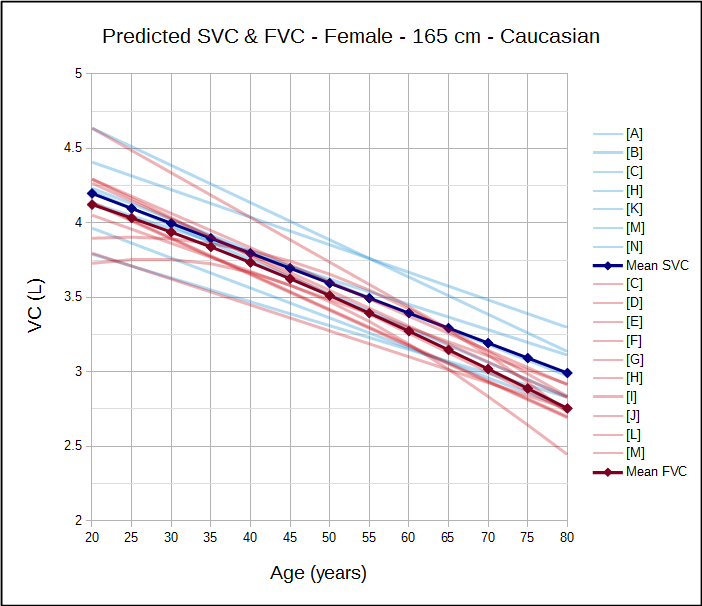
Having said that, an accurate FEV1/VC ratio is essential for detecting and quantifying airway obstruction and an SVC maneuver is more likely to obtain a more accurate VC. This matters because the current ATS/ERS spirometry guidelines recommend that the FEV1/VC be reported, where the VC is the largest value obtained from any test and reference equations indicate that the SVC is routinely larger than the FVC:
So, shouldn’t we be routinely performing both FVC and SVC maneuvers when we do spirometry on our patients? And why aren’t we?
Well first, although many test systems allow both FVC and SVC maneuvers to be performed relatively few of them will actually report the FEV1/VC ratio. The ATS 2017 reporting standards does mandate this, but here we are two years later and my lab has had no updates in our reporting software. If we want to report the FEV1/VC ratio we have to do so manually in the notes. This is a major hurdle that many are not willing to overcome.
Second, many clinics and doctor’s offices struggle just to perform adequate spirometry, nominally according to the ATS/ERS standards. There is frequently an additional struggle to understand what the results mean and simplistic algorithms are often used to make sense of them. Performing and using SVC measurements in this kind of environment is just too confusing to be considered, particularly since there is no mandate to use them.
Third, performing SVC as well as FVC maneuvers takes extra technician/patient time that just may not be considered to be available. I would argue that performing a shortened FVC maneuver optimized for FEV1 and SVC maneuvers optimized for VC will actually take little extra time but many (including the physicians I work with) would disagree.
Fourth, there very few good FEV1/VC ratio reference equations. There are only two studies (Gutierrez, Marsh) where FVC and SVC were studied in the same population and where a predicted FEV1/VC ratio can be calculated. All other reference equations, including the NHANESIII and GLI reference equations, can only produce a predicted FEV1/FVC. Since SVC is usually larger than FVC, this means that the predicted FEV1/SVC ratio is smaller than the FEV1/FVC ratio and it’s remotely possible that the presence of airway obstruction would therefore be overestimated. I would argue that SVC is accurate more often than FVC and that the FEV1/VC is therefore more likely to accurate more often as well.
Fifth and finally, there is no mandate to perform both FVC and SVC maneuvers. There is nothing in the 2005 ATS/ERS that says this should be done and SVC is almost always performed only when lung volume measurements are performed. Many if not most PFT labs hew closely to the ATS/ERS standards, and for good reason as this is the only way to be sure results are reproducible and transportable.
So although there are excellent reasons why both FVC and SVC should be routinely performed there are many significant obstacles towards doing so. To be honest my lab doesn’t routinely perform both maneuvers (despite my urging otherwise) and this is mostly because of reasons one, three and five.
Realistically it would take something like an updated ATS/ERS spirometry standard that mandated separate FVC and SVC maneuvers for this to become commonplace. Still, there will be select patients where getting a true VC and FEV1/VC ratio will be beneficial and we should be open to performing extra testing when it is needed.
Note: One work-around is to use the standard spirometry test module to perform an SVC maneuver. The FEV1 from the maneuver would be ignored and many test systems will allow the FEV1 and (F)VC from separate maneuvers to be combined and reported. We use this as needed in my PFT Lab.
Note: Very unofficially I have heard that the ATS/ERS will be releasing new spirometry standards sometime in 2019. I look forward to seeing them.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Standardisation of spirometry. Eur Respir J 2005; 26(2): 318-339.
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26(6): 948-968.
[A] Cordero PJ, Morales P, Benlloch E, Miravet L, Cebrian J. Static Lung Volume: Reference values from a Latin population of Spanish descent. Respiration 1999; 66: 242-250.
[B] Crapo RO, Morris AH, Clayton PD, Nixon CR. Lung volume in healthy nonsmoking adults. Bull Eur Physiopathol Respir 1983; 18: 419-425
Graham BL, Coates AL, Wanger J et al. Recommendations for a standardized pulmonary function report. An official American Thoracic Society technical statement. Am J Respir Crit Care Med 2017; 196(11): 1463-1472
[C] Gutierrez C, et al. Reference values of pulmonary function tests for Canadian caucasians. Can Respir J 2004; 6: 414-424.
[D] Hankinson JL, Odencrantz JR, Fedan, KB. Spirometric reference values from a sample of the general U.S. Population. Amer J Resp Crit Care 1999; 159: 179-187
[E] Johannessen A, Lehmann S, Omenaas ER, Side GE, Bakke PS, Gulsvik A. Post-bronchodilator spirometry reference values in Adults and implications for disease mangement. Amer J Resp Crit Care Med 2006; 173(12): 1316-1325
[F] Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow volume curve with growth and aging. Am Rev Resp Dis 1983; 127: 725-734
[G] Kuster SP, Kuster D, Schindler C, Rochat MK, Braun J, Held L, Brandli O. Reference equations for lung function screening of healthy never-smoking adults aged 18-80 years. Eur Respir J 2008; 31: 860-868.
[H] Marsh S, Aldington S, Williams M, Weatherall M, Shirtcliffe P, McNaughton A, Pritchard A, Beaseley R. Complete reference ranges for pulmonary function tests from a single New Zealand population. New Zealand Med J 2006; 119: N1244.
[I] Morris JF, Koski A, Johnson LC. Spirometric standards for healthy nonsmoking adults. Am Rev Resp Dis 1971; 103: 57-67.
[J] Morris JF, Koski A, Temple WP, Claremont A, Thomas DR. Fifteen-year interval spirometric evaluation of the Oregon Predictive equations. Chest 1988; 93: 123-27
[K] Neder JA, Andreoni S, Castelo-Filho A, Nery LE. Reference values for lung function tests. I. Static Volume. Braz J Med Biol Res 1999; 32: 703-717
[L] Pereira CADC, Sato T, Rodrigues SC. New Reference Values for forced spirometry in white adults in Brazil. J Bras Pneumol 2007; 33: 397-406.
[M] Roberts CM, MacRae KD, Winning AJ, Adams L, Seed WA. Reference values and prediction equations for normal lung function in a non-smoking white urban population. Thorax 1991; 46: 643-650.
[N] Stocks J, Quanjer PH. Reference values for residual volume, function residual capacity and total lung capacity. Eur Respir J 1995; 8: 492-506.