The 2005 ATS/ERS standards for assessing post-bronchodilator changes in FVC and FEV1 have been criticized numerous times. A recent article in the May issue of Chest (Quanjer et al) has taken it to task on two specific points:
- the change in FVC and FEV1 has to be at least 200 ml
- the change is assessed based on the percent change (≥12%) from the baseline value
The article points out that the 200 ml minimum change requires a proportionally larger change for a positive bronchodilator response in the short and the elderly. Additionally, by basing the post-BD change on the baseline value it lowers the threshold (in terms of an absolute change) for a positive bronchodilator response as airway obstruction become more severe. As a way of mitigating these problems the article recommends looking at the post-bronchodilator change as a percent of predicted rather than as a percent of baseline.
The article is notable (and its authors are to be commended) because it studied 31,528 pre- and post-spirometry records from both clinical and epidemiological sources from around the world. For the post-bronchodilator FEV1 and FVC:
- the actual change in L
- the percent change from baseline
- the change in percentage of predicted
- the Z-score
were determined.
The results were analyzed by various sub-groups and those for healthy non-smokers were interesting because they show the normal range of response to bronchodilators in a non-symptomatic population. Specifically the median post-bronchodilator increase in FEV1 was 0.071 L (+2.7% from baseline) while the median post-BD FVC showed a decrease of 0.019 L (-0.51% from baseline). The top 5th percentile (ULN) had an increase in both FEV1 and FVC of 0.32 L (+13.3% and +12.0% of baseline respectively). The bottom 5th percentile (LLN) was also instructive since it showed decrease in FEV1 of 0.118 L (-4.3% of baseline) and in FVC of 0.324 L (-9.5% of baseline) which is a reminder (which you will find on the product inserts when you read the fine print) that bronchodilators can cause bronchoconstriction in some individuals.
Since a bronchodilator response is most important for individuals with airway obstruction the results for sub-groups based on the degree of airway obstruction are particularly informative. For both males and females the greatest absolute change in FEV1 occurred in moderate and moderately severe airway obstruction (+ 0.240 L and + 0.242 L respectively) and was lowest in the very severe category (+0.155 L). The absolute increase in FVC however, increased as the level of airway obstruction increased, being lowest in mild obstruction (+0.070 L) and highest in individuals with very severe airway obstruction (+0.343 L).
When bronchodilator responsiveness was assessed using the ATS/ERS criteria for FEV1, the number of individuals who improved significantly was greatest in the moderately severe and severe categories (46.8% and 44.5% respectively for males and 27.1% and 26.8% for respectively for females) and lowest in mild and very severe airway obstruction (22.1% and 27.9% respectively for males and 23.2% and 16.0% for females).
FVC improvement on the other hand, showed that the post-bronchodilator change increased with the severity of airway obstruction, with the lowest increase in those with mild airway obstruction (4.0% for males and 4.6% for females) and largest in those with very severe airway obstruction (47.9% in males, 41.2% in females).
The article notes however, that one quarter of the subjects with a low baseline FEV1 (primarily elderly and children) had a >12% increase from the baseline FEV1 but that the increase was less than 200 ml. It also points out that the FEV1 increased by >12% from baseline in only 20% of individuals with mild airway obstruction but 55% of the individuals with very severe airway obstruction and that this change was inconsistent with the structural changes in the airways and the lung that occur in chronic airway obstruction (i.e. airways should be become less responsive as airway obstruction increases). For both these reasons the article recommends assessing bronchodilator response as a percent change of predicted (or the z-score) rather than from baseline.
The effect of this recommendation however, is that it decreases the number of individuals who would be considered to have a positive bronchodilator response, although this depends on the selected threshold. When compared to the current ATS/ERS criteria a 12% increase in percent predicted of the FEV1 causes the number of individuals with very severe airway obstruction to decrease from 27.9% to 7.0% in males and from 16.0% to 8.3% in females. When a threshold increase of 8 percent predicted in FEV1 is used (based on survival statistics from Ward et al) however, the number of individuals that show a positive response were 17.4% in males and 18.1% in females.
Interestingly, the increase in FVC based on 12% increase of the predicted FVC, although decreased from the ATS/ERS criteria, was still greater in individuals with very severe airway obstruction (28.7% in males, 24.1% in females) and lowest in individuals with mild airway obstruction (4.3% in males, 5.0% in females).
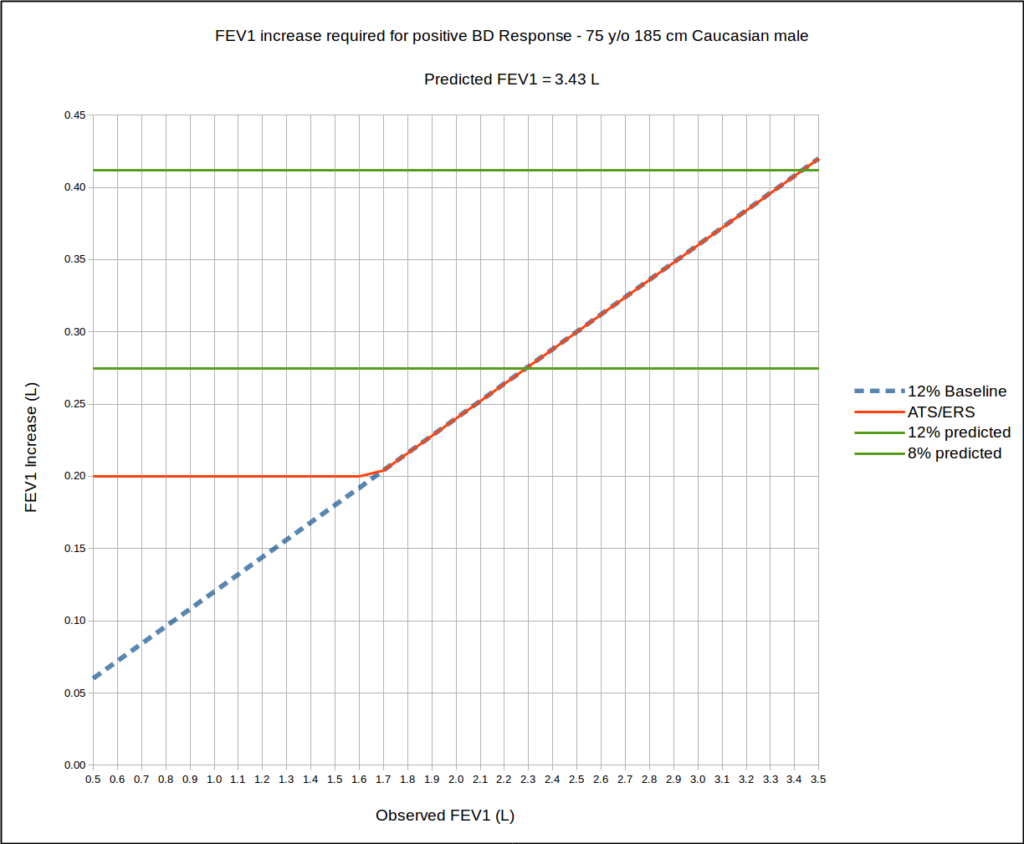
The effects of assessing changes in FEV1 as a percent of the predicted are less clear than might be initially expected. Using a 75 year old, 185 cm Caucasian male as an example, up until a normal baseline FEV1 of 100% of predicted, a 12 percent predicted change in FEV1 always requires a larger increase in FEV1 than does the ATS/ERS threshold. Using an 8 percent of predicted as a criteria however, up until a baseline FEV1 of 65% of predicted, the increase in FEV1 has to be somewhat larger than the ATS/ERS threshold but from 65% of predicted upwards, a significant change in FEV1 by 8 precent predicted is less than the ATS/ERS threshold.
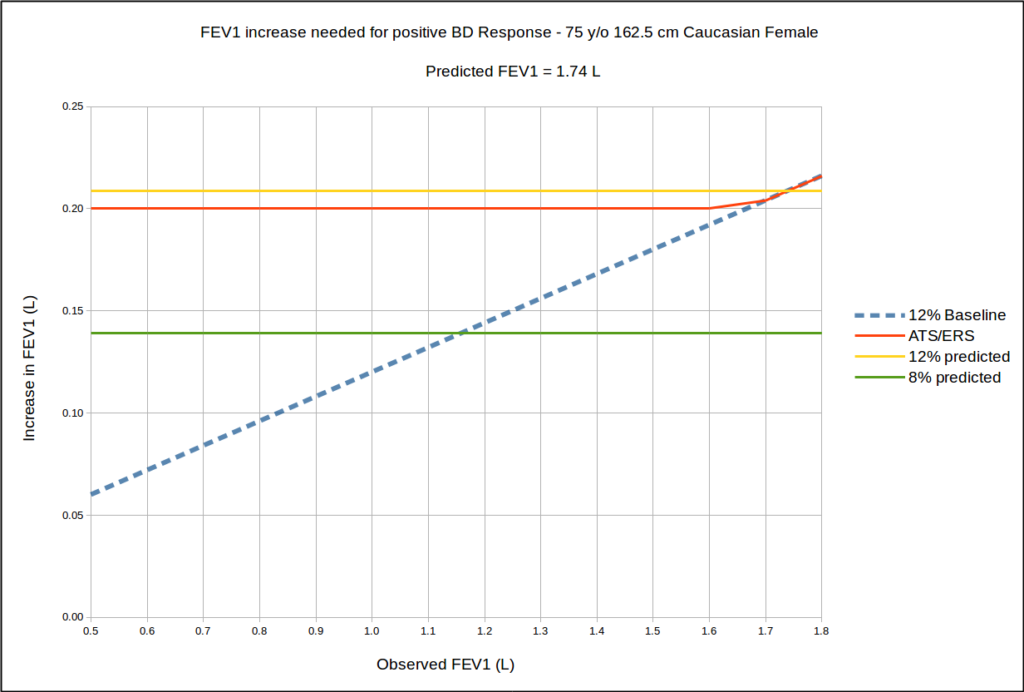
However, when a 75 year old 160 cm Caucasian female is used as an example, one of the problems of the ATS/ERS criteria becomes more evident since the 200 ml minimum is greater than a 12% increase from baseline until the baseline FEV1 is slightly greater than the predicted FEV1.
The article also points out the importance of changes in FVC in individuals with more severe airway obstruction. Most specifically, a much larger number of individuals with severe airway obstruction had a positive response to bronchodilator based on their increase in FVC than they did for FEV1. I am disappointed however, that the effect of expiratory time on FVC was not analyzed or discussed. Although a number of researchers have indicated that an increase in expiratory time is a clinically relevant effect of bronchodilators, changes in expiratory time and FVC have not been subjected to the same survival analysis that Ward et al made on FEV1.
It is past time that the ATS/ERS criteria for a positive bronchodilator response was updated and the findings presented in this article will likely influence the next ATS/ERS statement on interpretation (when and if it is published). Assessing changes in FEV1 and FVC based on a percent of predicted makes a great deal of sense, particularly since it does away with age and height biases imposed by the 200 ml threshold. The 200 ml threshold was based mostly on the need to differentiate a clinically significant increase from the “noise level” of poorly reproducible results but this tends to be influenced by a small number of individuals and as already noted makes no allowances for height or age. Comparing changes as a percent of the predicted makes a 200 ml threshold unnecessary.
In addition the 8% threshold for FEV1 advocated by Ward et al (discussed previously) appears to have a significant level of clinical relevance. Although the number of individuals considered to have a positive bronchodilator response would decrease in those with severe airway obstruction, it would increase in those with mild airway obstruction.
One final note is that the terminology involved in using a percent of the predicted is often confusing. It’s easy to get mixed up when you try to discuss FVC and FEV1 and then post-bronchodilator changes in FEV1 or FVC either as an absolute values or a percent of baseline or as a percent of predicted. In particular it becomes hard to say “there was a 12% increase in FEV1” without clarifying whether the increase is from the baseline or when compared to the predicted. Some standardization of the terms used would help clarify this. The authors bypassed this problem to some extent by frequently discussing the results in terms of their z-score but despite their underlying connection to statistics (and maybe because of it) z-scores are not as well understood as percent predicted and remain underutilized.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Interpretive strategies for lung function tests. Eur Respir J 2005(6); 26: 948-968.
Quanjer P, Ruppel GL, Langhammer A, et al. Bronchodilator response in FVC is larger and more relevant than FEV1 is severe airflow obstruction. Chest 2017; 151(5): 1088-1098.
Ward H, Cooper BG, Miller MR. Improved criteria for assessing lung function reversibility. Chest 2015; 148(4): 877-886.